1. Introduction
In 2019, with the approval of the Universal Health System, Sistema Único de Salud (SUS), Bolivia moved a step forward towards the achievement of universal healthcare coverage in compliance with its constitutional mandate that proclaims the fundamental right to universal and free healthcare access (National Political Constitution, 2009). Nonetheless, the approval of the reform has been controversial due to the multiple deficiencies that characterize the healthcare system. As outlined by the 2016-2020 Institutional Strategic Plan (PEI) prepared by the Ministry of Health (2017), the healthcare system was considered inefficient and inequitable due to fragmentation at the management level and to the insufficient response capacity of the health facilities that presented characteristics such as poor equipment, unmotivated professionals, lack ofHR and infrastructure, and low-quality services. The report also points to the lack of consideration of the population's cultural diversity in the provision of services.
Within this context, on the one hand, the implementation of Universal Health Insurance has been largely praised both domestically and at the international level for granting the possibility to 51% of the Bolivian population to access healthcare insurance. The World Health Organization (WHO) declared the Bolivian SUS as an ambitious health reform and as being “strengthened to withstand the impact of future health emergencies” (WHO, 2021). However, on the other hand, critics at home pointed to the precarious state of the health system; that is, to shortages in infrastructure, equipment and human resources that would be necessary to assist an additional 5 million Bolivians under the SUS.
The first visible effect of the SUS implementation has been a sharp increase in public insurance subscriptions. According to data released by the National Institute of Statistics (INE), subscriptions to public health insurance rose from 17.5% in 2018 to 52% in 2020. However, to date, there is little to no evidence available as to whether the massive registration corresponds to effective access, the nature and quality of the services granted under SUS, and the extent of its implementation.
The purpose of this study is to fill this research gap by analyzing the effects of the SUS on the access to public health services and to produce a diagnosis of the extent of access achieved, answering the following research question: How has access to public healthcare services evolved after the implementation of the SUS?
The research question has been addressed through an investigation based on combined quantitative and qualitative methods, relying on national statistics analysis and semistructured interviews with users, administrative staff, and other key stakeholders. Firstly, this study presents an evaluation of the healthcare system by analyzing data representative of access at the national level, obtained from the National Household Surveys of 2017, 2018 and 2019. Comparing dimensions such as effective access, availability, and affordability in the year prior and after the approval of the SUS allows for a first glance at the evolution of access to public services. Secondly, the macro perspective is integrated with a case study that provides a detailed analysis of the qualitative dimensions of access to healthcare.
Despite the case study not being representative of the entire national territory, the objective is not to generalize, but to collect revealing information about the qualitative dimensions of access to healthcare services. By doing so this study provides two fundamental contributions. It fills the existing research gap, by providing a general overview of how access to healthcare evolved after the SUS, through quantitative indicators representative of the national level. Secondly by comparing and contrasting the results from National Household Survey data with the case study, the study reveals information about healthcare access dimensions that are not reflected by quantitative data and that provide a richer picture of the opportunities and challenges involved in accessing healthcare. Third, the findings are also revealing and of interest to the wider national context. This is because the city of La Paz is among the municipalities receiving the greatest amount of financial resources1 and has one of the highest Human Development Indexes, scoring 0.719 in 2019 (Global Data Lab, 2019); making it unlikely for the findings to be outliers. On the contrary, it is likely for the challenges identified in the context of La Paz to be exacerbated in less resourceful areas. These hypotheses are to be verified by future studies.
To evaluate the SUS, the analysis employs a theoretical framework widely used by WHO (2010) that combines quantitative and qualitative indicators. The framework will guide the analysis for both the data representative of the national level and the case study.
The following section will summarise the main theories and available research. Subsequently, the methodology section will provide details about the methods used and the theoretical framework employed. Before proceeding with the analysis, a background section provides information outlining the general structure of the health system and the evolution of the public insurance system. Finally, the last section will present the results, first for the national level and then for the case study, after which a conclusion will summarise the findings and provide direction for further research.
2. Literature Review
The literature on universal healthcare access reflects the ongoing evolution in its conceptualization. In the 1970's, the focus was mainly on the structural factors of healthcare access, such as financial affordability and physical accessibility In these areas, many authors have highlighted that to achieve UHC, countries must raise sufficient public funds to cover the healthcare costs of those who cannot afford to contribute. In low-middle-income countries, where a large proportion of the population live on low wages and work in the informal sector, general government revenues are especially important. How to finance UHC in countries where the tax collection base is low is a topic particularly subject to debate. Reeves et al. (2015) stated in a study that pro-poor taxes on profits and capital gains seem to support expanding health coverage without the adverse effects of the outcomes observed for higher consumption taxes. In the context of low levels of formal sector employment, it is unavoidable that indirect taxes comprise a large proportion of tax revenue. Reeves et al. (2015) point out that whereas some indirect taxes (for example on luxury goods) are not likely to affect poor people adversely, and other indirect taxes might help improve health outcomes (for example taxes on tobacco and alcohol), other consumption taxes are highly regressive. Health-care user fees and co-payments, for example, represent a consumption tax on the sick that take countries away from UHC and adversely affect health outcomes.
Meheus & McIntyre (2017) show that a country's level of economic development does not predetermine its spending levels. In fact, they claim that increasing government revenue through taxation or other sources is first of all a fiscal policy choice. The mantra of lack of fiscal space can be challenged and government revenue can be increased through improved tax compliance and efficiency in revenue collection and increasing tax rates where appropriate. And, as argued by Matus-Lopez et al. (2019), there is a capacity to create fiscal space within the Bolivian health sector through economic growth linked to a commitment to reprioritize public spending on health, improvements in the internal sources of revenue through the reduction of informal work, and reduction of tax expenditures. The growth of Bolivia’s spending on health as % of GDP went from 4.6% in 2008 to 6.8% in 2016, showing that there can be fiscal space for health financing.
Additionally, ensuring a stable and sufficient government revenue can allow reducing the share of out-of-pocket spending, as Mills et al. (2012) argue. To abolish health user fees for some or all citizens is indeed a considerable way to improve access to healthcare. That is because “even tiny out-of-pocket charges can drastically reduce poor people's use of the needed services” as Yong Kim stated in 2013. The case for out-of-pocket spending preventing a considerable number of people from accessing services in Bolivia was documented by Coronado (2017), who showed that in 2016, of those that were sick and did not seek medical services (9.4%), did so due to lack of financial means.
An additional pillar of universal access is physical accessibility to healthcare resources. This refers to the availability of professional medical personnel, healthcare facilities, waiting and travel time. Otieno & Asiki (2020) propose some good practices at the level of service delivery to increase access to care. For example, to expand primary care services provided by community health volunteers (CHVs), community mobilization through the creation of support groups, and welfare organizations to spread health information, such as antenatal care and screening for chronic illnesses.
From the '80s onwards there has been a growing number of scholars (Penchansky & Thomas, 1981; Haddad & Mohindra, 2002) that identified multidimensional aspects ofaccess within the demand side, such as quality of care, cultural acceptability, need, and adequacy of healthcare services. In fact, Mooney (1983) points to the fact that access depends not only on factors of the supply side such as location, availability, affordability, and appropriateness of services but also on-demand factors such as knowledge of the individuals, practices of care and burden of disease. Similarly, Aday & Andersen (1974) state that utilization is defined by population characteristics and the health system's characteristics. Therefore, access to healthcare has been increasingly conceptualized as a process extending along a wide spectrum of factors involving qualitative and quantitative dimensions from both user's and supplier's sides.
Measuring the degree of universality in healthcare access might result in a complex procedure due to the variety of dimensions included in its conceptualization. However, through a good operationalization of the concept of access, empirical research might result in a good approximation of its status.
3. Methodology
3.1. Conceptual Framework
Access has been measured according to a widely used framework developed by the WHO (2010). The latter defines access as the opportunity to reach and obtain appropriate healthcare services in situations of perceived need for care, with access seen as resulting from the interface between the characteristics of persons, households, social and physical environments, and the characteristics of health systems, organizations and providers. The concept of universal health coverage is a multidimensional one, requiring multidimensional conceptualizations and metrics to be measured. In particular, both quantitative and qualitative metrics are needed to provide a comprehensive picture of the extent of universal health coverage in a given setting. The indicators outlined below are based both on quantitative and qualitative measurement methods, to produce a comprehensive picture of the change introduced by the SUS and of the overall status of the healthcare system when compared with its objective of achieving universality.
Effective coverage. The proportion of the population in need of an intervention who have received an effective intervention.
Availability The physical availability of healthcare, health infrastructure, workforce, medical goods and products, and timely provision of services. This is measured through physicians/nurses x 1,000, beds x 1,000, hospitals, geographical location /the location of a health facility will have an impact on access to healthcare depending on the patterns of settlement of the population it serves and their capacity to travel to the health service according to Levesque et al. (2013).
Affordability (of services). Is defined as the absence of financial barriers to needed healthcare aiming at avoiding health-related poverty or impoverishment. The affordability of services for individuals or households differs from fiscal affordability. It considers out-of pocket spending which is the amount of money a patient pays for medical expenses that are not covered by a health insurance plan. The macroeconomic affordability is the fiscal space that can be made to finance a level of expenditure that ensures universal access to services. It is measured as health spending as % of GDP and the percentage of investment in health as % of total public investment.
Quality. Refers both to the quality of infrastructure and the workforce to provide the healthcare services required (ILO, 2008). Access to healthcare is not only based on geographical aspects, organizational availability and affordability, but also on the user's possibility to choose acceptable and effective services.
3.2. Quantitative data analysis
The study has been conducted according to a combined methodology. First, analysis of quantitative data obtained from the 2016, 2017, 2018, and 2019 National Household Surveys, guided by the indicators of access, affordability and availability aimed at generating an overview of how access has evolved at the national level. The National Household Survey Data was collected by the National Institute of Statistics (INE) between January and December of the respective years through direct interviews with a total of 11,195 households in 2018 and 11,976 households in 2019 (INE, 2018, 2019). For this study, only section four of the surveys, about the topic of healthcare, has been analyzed. The sample is representative at the national level. Additionally, databases from the National Institute of Statistics (INE) and the Social and Economic Policy Analysis Unit (UDAPE) updated to 2019 have been used. The databases allowed to extract information related to households' socioeconomic characteristics, health services utilization, related expenses, and the system's availability of infrastructure and human resources. Secondary data obtained from National Household Surveys were analyzed with SPSS software, while data from INE and UDAPE was processed with Excel. The main analyses performed were descriptive and three-way tables.
Given that more and better information can be gained by converging the quantitative findings with qualitative information, the research was complemented by a case study In fact, the nature of the qualitative approach is to open the study by presenting the large, interconnected complexities of a situation (Creswell, 1999) which is precisely the objective of this research. To this end, semi-structured interviews have been conducted with health providers and users in the city of La Paz, to extend the findings of the first part of the analysis.
3.3. Qualitative data sampling
Data for the case study was gathered in the city of La Paz. The sampling strategy was based on a combination of convenience2 and purposive3 sampling. On the provider side, health center directors were interviewed, as they possess the highest amount of information about both the administrative and service provision sides of the health establishments. Additionally, to include as much variation in the sample as possible, health centers of different macro-areas4 of La Paz were selected according to the criteria that macro-areas are characterized by different levels of resources5 and assigned populations, hence diversity in dynamics of access. The areas selected were San Pedro, Sopocachi, Los Pinos, Cotahuma, La Merced, Macrodistrito Centro, Villa Pabón, and San Pedro Alto.
The users' sampling was guided by the criteria of age, gender and location of their assigned health center. As mentioned above, the location of a health center defines the nature of services due to their different levels of resources and thus quality, whereas differences in gender and age account for variation in experiences and perspectives.
3.4. Qualitative data collection and analysis
Both providers and users were recruited by direct contact in health centers and hospitals. A total of 6 health center directors were interviewed, with the saturation of information having been reached with this amount, while on the user side, 8 participants were interviewed, giving a total of 14 semi-structured interviews. Three users refused to be interviewed (one of whom after listening and reading the details about the study) without motivating their choice. The interviews held in the city of La Paz, lasted between 20 and 30 minutes and were recorded with a digital recorder. One participant preferred not to be recorded.
Before the start of the interview, all participants received both oral and written information on the purpose of the research, its methods, use of data and privacy policy, as well as on the voluntary nature of participation and the right to withdraw at any moment. They all signed written consent to participate in the study. The interviews were held between November and December 2021. The table below illustrates the main questions guiding the semi-structured interviews. The questions were generated after the quantitative analysis part of the study was concluded, the results of which guided the development of the questions.
Table 1 Interview questions
| Health providers | Users |
|---|---|
| To what extent has the number of users at this health center increased after the approval of SUS? | What do you think about Universal Health Insurance? |
| What type of services does the SUS cover? | What services does the SUS cover? |
| Were the resources provided to this health center sufficient for satisfying the increase in demand? | How do you think the quality of public health services has evolved in the first year of implementation of the SUS? |
| To what extent has the approval of SUS eliminated the economic barrier to accessing healthcare? | Do you think there is sufficient information regarding the SUS? |
| What were the consequences of increased demand in terms of the quality of the services? | What are the major benefits and the major challenges encountered under SUS? |
Source: Prepared by author, 2021.
The data collected through interviews were transcribed and analyzed according to coding and thematic analysis methods. The codes were first organized into broad categories according to the theoretical framework used. The analysis identified patterns of association in codes or themes across cases, and between sets of codes in the data. The codes were repeatedly revisited and adapted throughout the analysis process.
3.5. Limitations
One of the study's limitations concerns the fact that while the study's purpose is to perform a diagnosis for the first year of SUS implementation, that is, in 2019, the interviews were conducted in 2021. To counter this limitation, before beginning the interviews, the interviewer asked the participants to relate their answers to the year 2019. Clearly, it is not possible to know the extent to which the participants were concise in reporting experiences solely about that year. However, the validity of the data is guaranteed by the fact that previous research confirms the existence of the issues identified with the interviews (2016-2020 Institutional Strategic Plan, Ministry of Health, 2017; Chacon & Valverde, 2009; Narvaez & Saric, 2004), thus confirming that the deficiencies identified are not a product of the pandemic but existed before it.
Another limitation is related to the data sampling methodology. Limited resources and time made convenience sampling the most adequate method for this study Nonetheless, the problem with convenience sampling is the high probability of underrepresentation or overrepresentation of particular groups. In this study, the risk might be that users' negative experiences be overrepresented and positive ones be underrepresented. However, given that the findings that emerged in the case study on the healthcare system deficiencies correspond to similar previously studied and reported cases, and the quantitative indicators of the analysis, it is unlikely for this bias to have had a considerable impact on the findings.
4. Background
4.1. Historical context
Salazar & Rocha (2020) provide a quick historical recap on the Bolivian health system. In Bolivia, the first health system emerged in the 1930s. It was an elite system excluding the vast majority of the population. In the 1950s, after the National Revolution, a social security system was created for formal workers, leading to the establishment of the National Social Security Fund - Caja Nacional de Seguridad Social- in 1953. Subsequently, the social security system went through an intense process of fragmentation, with the generation of several other health funds, reaching a total of 16 different health funds with more than 40 medical health insurances, autonomous administrative capacity, and no degree of coordination with each other (Bermudez et al, 1999; Tejerina, 2018).
By the 1980s, after the Alma-Ata Declaration (1978), a program targeting broad immunization was implemented in Bolivia, and the health system was partially regionalized (Tejerina, 2018). In 1994, with the introduction of the Popular Participation Law, the ownership of public health infrastructure was given to municipal governments. In 1996, the government approved the National Health Insurance for Maternity and Children (SNMN) scheme, to improve maternal health and reduce infant mortality (Muriel, 2007). This insurance scheme was redefined in 1998 as Basic Health Insurance, emphasizing access in rural areas. Finally, in 2003, the Universal Maternal and Child Insurance (SUMI) was implemented, substituting the previous ones and granting free and universal services to pregnant women until six months after childbirth and to children up to the age of five (Muriel, 2007). In January 2006, the government created the Health Insurance for Older Persons (SSPAM) scheme through Law N° 3323, which conserves the coverage of benefits established in the Free Health Insurance for the Elderly, but with modified financing, depending on municipal funds from the Direct Hydrocarbons Tax (RAF, 2006). In 2008, the government established, through Supreme Decree (SD) N° 29601, the Healthcare and Management Model, in the framework of Intercultural Community Family Health (SAFCI), to eliminate social exclusion and promote social participation. In 2013, SIS (Servicio de Salud Integral) was approved, unifying and expanding SUMI and SSPAM (for more information, see Muriel, 2007). On February 27th, 2019, SD Nº 3813 established the implementation of the SUS, to provide a universal, public and free health system for approximately 51% of the population (5.8 million people). Within this framework, the SUS began its rollout on March 1st, 2019.
4.2. The legal foundations of the fundamental right to universal healthcare
The first Bolivian Constitution to include health as a responsibility of the State was that of 1938. The fundamental right to health was proclaimed in the Bolivian Constitution of 1967 and was further reinforced in the more recent 2009 National Political Constitution. The latter dedicates an entire chapter to the topic (Chapter II), made up of eleven articles that proclaim the duty of the State to guarantee free and universal access to healthcare without any discrimination (Article 18), to provide a sole universal, free and equitable health system (Article 18, II), to promote public policies to reinforce this right, and to monitor the quality of the service through the monitoring of the human resources, infrastructure and equipment (Article 39).
4.3. The Bolivian healthcare system
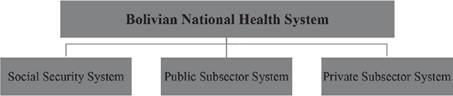
Currently, the Bolivian health system consists of a public and a private sector. The public sector is divided into two subsystems: the social security system and the public system. The three subsectors share a high degree of internal fragmentation and segmentation (Tejerina, 2018).
One of the public subsystems is a contributory one, the social security system -seguridad social- that operates through health insurance funds -cajas de salud- to which the employers from the private sector and public institutions, subject to the labor laws, contribute 10% of their salaries. In Bolivia, there are several health insurance funds: Caja Nacional de Salud, Caja Petrolera de Salud, Caja de Caminos, Caja de la Banca Estatal, Caja CORDES, SINEC, Caja de la Banca Privada, COSSMIL (military), and the university insurance. The National Health Insurance Institute (INASES) is responsible for this section of the public health system, particularly of implementing, controlling and supervising the policies and norms related to health insurance (Medrano, 2006).
On the other hand, the non-contributory insurance system, headed by the Ministry of Health and Sports (MSD) covers with its public resources the population that cannot access contributory-based insurance. The public subsector is financed with public funds allocated to municipalities (20% of central government tax revenues) and uses MSD infrastructure (Muriel, 2007). The Bolivian public healthcare system has four levels of management (national, departmental, municipal, and local), that provide each part of the financial resources and administrative capacity for the public healthcare system. The central level finances the human resources (HR) of the public subsector with funds from the General Treasury of the State and has administrative capacity across the four levels. As Tejerina (2018) highlights, in practice, in public health establishments, besides HR financed by the State, there is also HR contracted by the department and municipality, resulting in dispersion and inefficiency in service delivery The 339 municipalities are in charge of administrating first and second- level healthcare services, while the nine departments administrate the third levels. The health products of the first and second levels are financed through 15.5% of the tributary sharing or the equivalent of the IDH (Law N° 1152, 2019). The different elements of the health system are not articulated and coordinated with each other, leading to overlaps and gaps. Fragmentation inevitably leads to ungovernability and inefficiency (Tejerina, 2018).
Lastly, the private sector is divided into for-profit organizations (insurance and private services and clinics) and not-for-profit organizations (NGOs and the Church).
4.4. SUS beneficiaries & benefits
According to Article 5, Chapter II of the legislative text of Law N° 1152, the beneficiaries of universal free healthcare are:
a) Bolivians who are not covered by social security insurance;
b) foreigners that are not covered by social security insurance or who belong to the categories of pregnant women, women in need of sexual and reproductive assistance, children less than five years of age, men and women older than 60, and people with classified disabilities.
People belonging to these categories can register at the nearest first-level health establishment, by presenting their ID and one of the most recent water, electricity or gas bills.
In total there are 1,200 services in 250 packages that are free for SUS subscribers and that were previously subject to a cost for 63% of the population that lacked health insurance subscriptions. The Ministry of Health stated that progressively SUS would reach complete free coverage of health services. Additionally, the list of services is not exhaustive and if health personnel can grant additional services not mentioned in the list, it is not limited to doing so.
At the first level, the health services include all services necessary for the following categories: health promotion and disease prevention, diagnosis and rehabilitation of diseases, medical and odontological consultations, nursery services, vaccines, medicines, medical supplies, laboratory and office exams etc. (Health Ministry, 2019).
The second and third levels of care include specialized medical attention, hospitalization, medicines, medical supplies, services complementary to the attention of the patient, laboratory and office exams, blood tests, and others of a similar nature.
The law as well as health centers' directors emphasized the disease preventive function of the first level, which is not provided with specialist doctors, and requires a transfer to the second level of healthcare for specialized diagnoses or treatments. Similarly, at the second level, hospitalization and some surgeries are included in the treatment needed for several diseases.
Article 7 of Law N° 1152 establishes the rules for access to healthcare services. Persons in need of health services must access them through the first level of care. In fact, 80% of cases can be theoretically resolved at the first level of care, thus avoiding overdemand for services at the second or third levels and consequently a collapse of hospitals with limited human and physical resources. It is thus crucial for these resources to be employed for the cases that truly require them.
5. SUS: Dimensions of Access to Public Healthcare Services
5.1. Who are the beneficiaries of the Universal Health Insurance scheme?
Coverage refers to the population eligible for a set of healthcare services or packages. With the approval of the SUS, the first visible change has been in the total amount of subscribers to the public insurance scheme.
While in 2018, the subscribers to the public insurance schemes was 18%, and the ones declaring not being affiliated with any health insurance scheme was 63%, these figures have considerably evolved with the approval of the universal healthcare scheme. In fact, data from the National Institute of Statistics (INE) shows that in 2019, 46% of respondents reported being affiliated with the SUS, while the percentage of respondents declaring not being affiliated with any insurance scheme dropped to 34%. As the graph above shows, the subscriptions to the public healthcare scheme have undergone a considerable evolution in 2019 compared to previous years (figure 2).
As to the geographic distribution of the SUS's affiliates, it shows a high concentration of rural subscribers. In fact, according to the latest statistics released by INE, while in 2018 only 22.97% of rural respondents declared being affiliated with the public insurance scheme, the percentage reached 71.6% in 2019. On its part, the urban population in percentage went from 15.2% in 2018 to 35% in 2019. While urban subscribers more than doubled, the more remarkable change has been among the rural population. Data also indicates that among subscribers, women are slightly more numerous (25%), compared to men (21.08%) (INE, 2019).
Additionally, the median household income of those affiliated with the SUS is about 810 bolivianos per month, slightly higher than the 788 Bs./month in 2018. Before SUS there was still a considerable proportion of the population not covered by any type of health insurance. Typically, those excluded were adolescents and adult men that did not have formal employment and were thus not entitled to any of the health fund insurance schemes, having to pay out of their pockets for healthcare services.
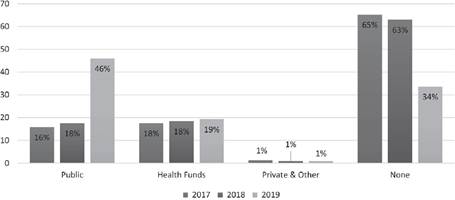
Source: Prepared by author, with data from INE (2019) 6.
Figure 2: Bolivia: Total population registered under health insurance, by sector, 2017, 2018 and 2019
Coronado (2019) shows that in 2016 those who did not manage to access health services, were the adult groups (especially when there were money constraints), heads of household, and lived in rural areas. Also in this group were adults who did not have regular education and those who did not complete primary school. Particularly, in 2016, among the reasons for not seeking healthcare, 9.4% declared economic reasons (Coronado, 2019). It might be hypothesized that on the one hand, SUS offered opportunities for accessing healthcare for the disadvantaged groups previously excluded from health services. On the other hand, as Coronado (2019) notes, it is also possible that the economic crisis is widening informality rates, thus groups previously covered by the corto plazo (short-term) insurance lost it, especially in urban centers.
Table 2 Household income per capita (Bs./month) of subscribers to public health insurance, 2018-2019
|
Subscribers to SIS (2018) and SUS (2019), income in Bs./month |
2018 | 2019 |
|---|---|---|
| Mean | Bs. 1,010.30 | Bs. 1,014.20 |
| Median | Bs. 788.10 | Bs. 809.90 |
| Mode | Bs. 300.00 | Bs. 500.00 |
Source: Prepared by author, with National Household Survey data, 2018-2019.
As debated widely in the literature, an important question in healthcare access is to determine whether formal coverage corresponds to effective access. The next session will thus present the results and discuss the extent of effective access to universal healthcare services.
6. Effective Access
The latter is defined as the share of the population in need of an intervention that effectively received it. The definition of access is complex and multidimensional. Once having identified the population with health issues, it might be that a person in this group does not perceive the need to seek medical attention, and decides to not seek medical attention for several reasons or that outcomes of the health service received are unsatisfactory
In this paper, access is identified as the share of population that have reported health issues in the previous twelve months and have sought health service in a public health establishment, independently of the outcome of the service. The limitation of this measure lies in not knowing the reasons for those that were sick and did not go to any health service.
According to National Household Survey data, in 2019, among those getting sick, 62.1% went to a public health entity, compared to 46.8% in 2018 and similar values in previous years. In the years analyzed, less than half of those reporting an illness used a public health service, either because they considered it unnecessary, because of supply-side barriers or preference for private health services. Moreover, service utilization across the income spectrum shows 35% of the first and second poorest quintiles using public health services between 2016 and 2018, while for the third quintile, it is 30%. In 2019, around 41% of the two poorest quintiles that got sick used public health services. Additionally, between 2016 and 2018, among those reporting health issues and having visited a public hospital, roughly 58% did not possess any type of health insurance, a percentage which in 2019 decreased to 21.4%.
Table 3 Percentage of population reporting illness that attended health services in the previous 12 months, 2016, 2017, 2018, and 2019
|
% Getting sick and attending public health establishments |
2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|
| Yes | 52.8% | 53.7% | 46.8% | 62.1% |
| Poorest | 36.1% | 32.2% | 35% | 41.0% |
| 2nd quintile | 33.6% | 30.8% | 34.8% | 40.3% |
| 3rd quintile | 31.2% | 30.6% | 30.6% | 33.9% |
| 4th quintile | 27.9% | 25.1% | 27.1% | 29.5% |
| Wealthiest | 21.3% | 19.8% | 21.7% | 20.9% |
| Public insurance | 33.7% | 29.4% | 34.8% | 73.6% |
| Not insured | 58.5% | 58.3% | 57.8% | 21.4% |
Source: Prepared by author, with National Household Survey data, 2016, 2017, 2018, and 20197.
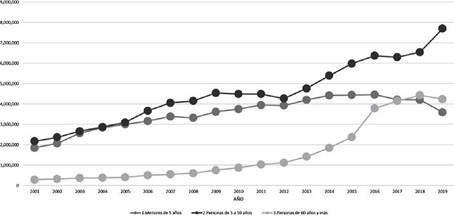
Another indicator that points to an increase in effective access is the number of outpatient visits in the public subsector reported by the National Health Information System for Epidemiological Surveillance (SNIS-VE) and the Ministry of Health and Sports (MSD) for 2019. This indicator shows a general growing trend in the number of outpatient visits within the 5-59 age group, with an evident surge from 2018 to 2019. The latter age group corresponds, except for pregnant women, to the category that was not covered by any of the previous public health insurance schemes 8. As to the >60 age group, until 2018 it showed a steady increase in the number of outpatient visits, probably due to the provision of the nutritional supplement CARMELO9 approved in 2015, for 2019 we see a slight downward trend compared to previous years.
The growing trend in accessing health services is also reported in a recent study by Coronado (2020). The findings indicate that in general, of the 18,000 adults in the National Household Survey that reported health issues in the previous 12 months, 70% accessed some type of medical attention. In particular the opportunity curve for medical attention turned out to be 84% in rural areas and 67% in urban areas. The study also reports that in 2019, the three poorest deciles have advantages in accessing medical attention, compared to previous years.
While formal coverage, outpatient visits, as well as the opportunities for accessing healthcare for the poorest quintiles of the population have increased according to statistical data, it is important to elucidate the type and nature of the services to which patients have access through SUS. To this end, the information gathered through qualitative data provides a clearer perspective on the nature of the services patients have access to.
7. Affordability
Affordability is measured through out-of-pocket spending and macroeconomic indicators (WHO, 2010). The latter is measured through health spending as a percentage of GDP, per capita spending, and percentage of public investment in the health sector. Effective universal financial protection can be attained not only if the population does not incur substantial out- of-pocket (OOP) payments and critical income losses due to payment for healthcare, but if there are no fears of and delays in seeking healthcare due to financial reasons, no borrowing and sale of valuable assets to pay for healthcare, and no detentions in hospitals for nonpayment of bills.
7.1. Out-of-pocket spending (OOP)
According to National Household Survey data presented above, there is an increase in the utilization of public health services compared to previous years. However, when it comes to out-of-pocket spending11, the median value for 2017, 2018 and 2019 appears to be roughly the same. Similarly, in breaking down the indicator into its various components, the median spending for outpatient visits was Bs. 100 for 2018 and Bs. 126 for 2019, thus presenting a slight increase in 2019. Only when it comes to expenditures on laboratory analyses or ambulances, in 2019 the average spending was half the one of 2018. As to medicine, it presents the same value for both years, at Bs. 80 (National Household Survey, 2018, 2019).
Table 4 Household out-of-pocket spending per year, 2017, 2018 and 2019
| Out-of-pocket spending (OOP) Bs./year | 2017 | 2018 | 2019 |
|---|---|---|---|
| Mean | Bs. 626 | Bs. 333 | Bs. 334 |
| Median | Bs. 110 | Bs. 100 | Bs. 100 |
| Mode | Bs. 50 | Bs. 50 | Bs. 50 |
Source: Prepared by author, based on National Household Survey data, 2017, 2018 and 2019.
Additionally, WHO's Global Health Expenditure Database reports that in Bolivia, in 2018, OOP was 22% of total health expenditure, while in 2019 it was 23.87%. The same source informs that domestic government expenditure went from 72.8% of current health expenditure (CHE) in 2018 to 71.2% in 2019. Why is the median OOP expenditure almost unchanged between 2018 and 2019, and why has OOP as a share of current health expenditure increased? Did public providers refuse to lower or abolish user fees? Is it that universal insurance covers only a basic package, making people still have to pay for services? Or is it that services are of low quality, making people go to private providers when they need quality service, hence the same spending levels?

Figure 4: Domestic government expenditure and out-of-pocket expenditure (OOP) as % of current health expenditure (CHE), 2019
Interviews with users and providers reveal that the OOP expenditure can be explained in the case study by a combination of the above-mentioned factors. Nonetheless, even if out- of-pocket spending values are constant, it is important to check the evolution of catastrophic spending. In fact, under universal health coverage, people might have the same out-of-pocket expenses, but less risk of impoverishment compared to previous years (Grogger et al, 2015). It is therefore important for future research to monitor the evolution of catastrophic health expenses, given and considering that they can also constitute relatively small payments for households close to or under the threshold of the national poverty line (WHO, 2010).
7.2. Macroeconomic affordability
The health expenditure concerning GDP increased moderately. In 2010, health spending was 5% of GDP and in the following year it reached 7%, but then fell again to 6% in 2017, and finally reached 6.9% in 2019 (WHO Data, 2019), placing Bolivia in the 19th position in health expenditures as % of GDP of countries in Latin America and the Caribbean (Statista, 2021). When the SUS was approved, experts called for an increase up until 10% of GDP in health spending to be able to support the system. However, health spending for 2019 stayed roughly unchanged compared to 2018. Although health spending growth was more than double the average rate for the region (OECD, 2020), Bolivia has low spending on health compared with neighboring countries.
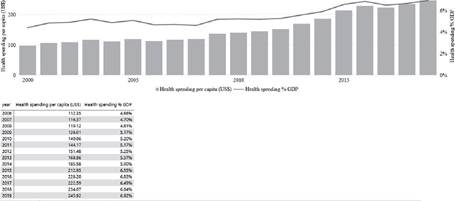
Source: WHO, Global Health Expenditure Database, 2019.
Figure 5: Current health expenditure (CHE) as % GDP and CHE per capita, constant US$, 2019
Health expenditure per capita per year in constant US$ has also slowly increased from year to year, having more than doubled since 2010. In 2019, current health spending per capita was US$ 246, an increase of only US$ 11 compared to 2018 (World Health Organization Database, 2019). Given the present health spending levels, Aponte et al. (2019) state that the required per capita spending to sustain universal health coverage in Bolivia should be US$ 400.
On the other hand, health expenditure as a percentage of general government expenditure increased only 2 percentage points in the last decade, from 10% in 2010, to 12% in 2018 (WHO, 2018). Similarly, investment in health for the year 2018 was US$ 264,035, whereas in 2019 it was US$ 293,058 dollars, out of US$ 500,000 programmed, constituting 7.7% of total public investment (Ministry of Economy and Finance, 2019). Although there is no straightforward answer to the question of how much a country should spend on health, the answer depends on a variety of factors, such as the health problems a country faces, the effectiveness of the existing health services, the price of inputs, and the priority in the allocation of funds, among other elements (Savedoff, 2007). Although there are slight improvements when it comes to Bolivian health expenditures, the data indicates that the government must ensure a broader and more efficient flux of resources at the macro level to its healthcare system to reach the conditions typical of a universal health system. To make the case more explicit, the tables below present the typical values of some indicators under Universal Health Insurance, comparing them with the ones in Bolivia.
Table 5 Economic indicators under universal health insurance and Bolivia
| Indicators | Universal | Bolivia |
|---|---|---|
| % of GDP spent on health | ≥ of 10% | 6.4% |
| Public spending as % of total health spending | 75% to 100% | 71% (WHO) |
| Current health spending per capita | US$ 3,994 PPP13 | US$ 496 PPP |
Source: Prepared by author, with data from Aponte et al. (2019), World Bank (2018) and WHO (2019).
| Indicators | Universal | Bolivia |
|---|---|---|
| Life expectancy at birth | ≥ 75 years | 71 years |
| % of population living under poverty line | 0 to 20% | 37.2% (WB) |
| Infant mortality rate (per thousand) | 0 to 6 | 21 (before first year after birth) |
| Maternal mortality rate (per 100,000 livebirths) | ≤ 20 | 155 per 100,000 livebirths (WB) |
Source: Prepared by author, with data from Aponte et al. (2019), World Bank (2018) and WHO (2019).
8. Availability
In 2019, the government promised an investment of US$ 200 million, for the hiring of 8,000 new human resources and to provide for the construction of new hospitals. It was said that the process would be gradual and step-by-step. However, at the end of 2019, there were few additional resources.
According to data from INE, in 2019 there were in total 3,983 health establishments in Bolivia: 3,610 first-level health centers, 238 basic hospitals, 47 general hospitals, and 32 specialized institutes which provide third and fourth-level care. In 2019, there were 55 additional health structures, compared to 2018, the majority of which were primary health centers. The graph below shows the distribution of health structures across Bolivia in 2019.
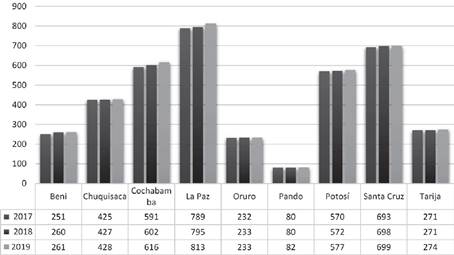
Source: Prepared by author, with data from UDAPE (2017-2019)14.
Figure 6: Total health establishments in the public subsector, by department, 2017-2019
It shows that the departments of Beni, Pando, Oruro, and Tarija have seen zero or two additional health establishments, despite being the departments where access to services is the most challenging, thus needing the most investment. Critics however claim that many of these new health establishments are not functioning, as they lack the necessary equipment and human resources to be operative. Similarly, others claim that the construction of many establishments is incomplete. Marconi (2021) suggests that it is necessary to carry out an external, technical, and financial audit, and to review the distribution with sector specialists and financial auditors, since there are voices that claim that the choice of locations was mostly for political and clientelist reasons. The distribution of health structures plays a very important role in access to healthcare. In fact, the location of a health facility will have an impact on access to healthcare depending on the patterns of settlement of the population it serves and their capacity to travel to the health service (Levesque et al., 2013).
Similarly, with regards to hospital beds available in 2019, there were an additional 633 beds compared to 2018. The additional beds make for an average of 2.09 beds per 1,000 inhabitants in line with the LAC average, but below the values of eleven countries in LAC and below the OECD average of 4.7 per 1,000 inhabitants (OECD, 2020).
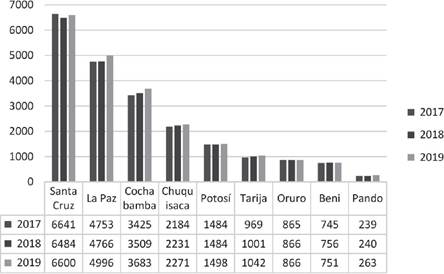
Source: Prepared by author, with data from UDAPE (2018-2019)15
Figure 7: Total available beds, by department, 2017, 2018 and 2019
However, the level of inpatient services required by individual countries depends on several factors and there is no global target for the number of hospital beds per country (WHO, 2018). Moreover, the total number of beds per department has increased mostly in Santa Cruz, La Paz and Cochabamba, leaving the other departments -which are the ones with less resources- with almost the same quantity of beds.
As to human resources (HR), the latest available data indicates that in 2019 there were an additional 2,493 human resources compared to 2017 in the public subsector (UDAPE, 2019). In 2019, there were 1.06 doctors per 1,000 people and 1.3 nurses and auxiliary nurses per 1,000, which is far below the 2.1 LAC average (OECD, 2020), and below the threshold of 4.45 skilled health workers (physicians and nurses/midwives) per 1,000 inhabitants to deliver on the ambitions of universal health coverage (WHO, 2016). The data indicates that the 2019 increase in human resources supply does not considerably change the ratio of HR per thousand inhabitants. Moreover, the average at the national level does not reflect the inequality in the distribution of HR, thus not reflecting the real availability in areas with less resources, especially rural ones.
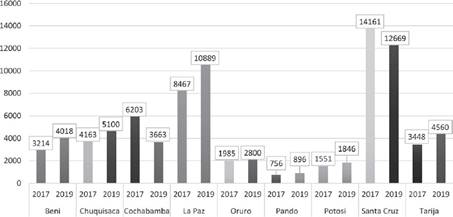
Source: Prepared by author, based on data from UDAPE (2019).
Figure 8: Total human resources in the public subsector, by department, 2017 and 2019
As the data disaggregated per thousand inhabitants reveals, the additional resources provided for the first year of the Universal Health Insurance implementation have generated a small relative improvement compared to previous years. That is because the new health establishments and beds of the public subsector have been provided mainly for the major departments of La Paz, Santa Cruz and Cochabamba, while the rest remained with roughly the same number of resources. Similarly, despite the supply of new human resources in the public subsector, when considering the availability per 1,000 inhabitants, the values continue to be below the LAC average and WHO recommendations, generating doubt as to the extent of lack of HR in public health establishments.
9.Access to SUS healthcare services: a case study of La Paz
In the following section, the analysis is broadened by reporting qualitative data guided by the indicators used in the first part of the analysis and by adding the dimension of quality. As mentioned in the methodology section, the objective of the case study is to open up the analysis to aspects that are not necessarily reflected by the quantitative data and to have an overall understanding of access dynamics in the city of La Paz. Moreover, the case study could be useful as a comparative metric to formulate hypotheses for future research into national contexts.
9.1. Effective access
At the first level of healthcare, users and center directors confirmed the gratuitous nature of consultations and basic medicine provided under SUS. However, interviewees complained that the medicine covered by the SUS at the primary level of healthcare is basic, such as paracetamol and ibuprofen, whereas when it comes to more expensive medicine, this is not covered or not available. Additionally, many patients and health center directors reported that there are cases in which also basic medicine lacks. In fact, all interviewees, except one, reported having experienced at least one shortage of medicine at their health centers. Additionally, all interviewees expressed a well-known and long-standing characteristic of the health system, that is, the long waiting times that require patients to wake up very early in the morning and to wait several hours if not the whole day to get access to a consultancy. Furthermore, the sheets that authorize consultations for a given day are limited, meaning that if a patient does not arrive early enough at the health center, they might not get a sheet for that day, having to come back on the following day With the approval of the SUS, the dynamic of long waiting times has been exacerbated due to a notable increase in demand.
With regards to the second level of care, coverage includes hospitalization, surgery and medication. The first difficulty in accessing secondary-level specialized care, according to patients, come from the fact that is difficult to get a transfer to specialized hospitals and that the long waiting times at the primary care level imply that patients' health condition can deteriorate during the waiting period. On the other hand, health center directors reported that the challenges arise from the fact that coordination with the second level occurs through a third center that coordinates the transfers. Sometimes the center does not respond to calls or reports a lack of availability of beds, so the director cannot approve the transfer and the patient can't access specialized public healthcare, leading to resorting to private health services (when the patient can afford it). Additionally, second-level directors declared receiving references for cases that can be dealt with at the first level of care. An ulterior challenge comes from the fact that hospitals have difficulty in providing health centers with counter-references16, weakening the fundamental right to continuity of care. These limitations hinder the quality and extent of effective access to specialized levels of care.
9.2. Out-of-pocket expenditure
Health center directors lamented shortages in medicines. Interviewed users and directors revealed that as a consequence of the lack of medicine at health centers, patients had to pay for them. Some of the health center directors reported that in some cases patients had to pay even for the paper on which to print their receipts, due to the lack of paper and printer capacity at health centers. Some users also complained that SUS does not cover complex medicine that requires out-of-pocket spending. Also, quality issues such as long waiting times lead users who can afford it to resort to private health centers, thus increasing out-of-pocket spending.
This partly explains the fact that OOP did not decrease between 2018 and 2019. Another explaining factor is the perception that users have about public healthcare. As reported by health center directors and users, there is a widespread perception that public healthcare services are of low quality, due to insufficiency of equipment, HR, and infrastructure, and also, according to users, due to bad treatment from doctors and nurses towards patients, especially towards those coming from rural areas. As reported in other studies in the literature (WHO, 2018; Atun et al., 2015), when there is a perception of bad quality, users prefer to spend out of their pockets to get quicker and more efficient health services. Moreover, some patients reported that in some cases the medical staff itself recommends patients go to private centers, as transferring them to the second level of care may require several days or weeks of waiting. One of the interviewees reported that when her mother got sick there were no available beds in the public hospital where she went, forcing her to resort to a private clinic for treatment.
Finally, another explanation might be the fact that OOP might not decline immediately with Universal Health Insurance, with the reasons being, among others, that before the existence of the insurance scheme, households used to not spend or spent less on healthcare services, as Grogger et al. (2015) showed from analyzing Mexico’s experience with universal healthcare.
9.3. Challenges at the macroeconomic level
As already mentioned, the law stipulates that 15.5% of the coparticipacion tributaria (tax coparticipation) is given to the first and second levels of healthcare. In addition, this budget can be increased or added to with other financing sources. An official working for the municipal secretariat reports that the 15.5% as a budget is far from sufficient. First of all, she reports that the services that cannot be covered by the third level are covered by the second level, putting additional pressure on the system. Secondly, the distribution of resources is done according to the population. However, many people that use the services were not present at the moment of the census, due to migration phenomena, thus generating a permanent deficit in terms of resources per capita. Besides, resources from international organizations have also been gradually diminishing. Another deficiency arises as bigger hospitals receive more resources. However, the official states hospitals with low-quality services and the first levels of care should receive more funds. The fragmentation and the different bodies in charge of management make it difficult for the municipal level to be efficient, she reported. Overall, the scarce financial resources provided by the Ministry of Health constitute a challenge for the adequate provision of services and there is no single, coherent and applicable financing model at all levels of management to ensure equitable distribution of resources.
The fragmentation of the healthcare system implies different degrees of responsibility for the scarce functioning of the system. Further investigation must be done concerning the different levels of responsibility, as the municipal level complains of receiving insufficient resources, while the central level points to weak administrative capacity in the departments and municipalities. It seems that among the different bodies that make efforts to manage the healthcare system, none is fully successful as the internal bureaucracies do not support them, there are no effective tools to coordinate among each other, and the mechanisms for social participation and control are insufficient (Tejerina, 2018).
9.4. Availability
Health center directors interviewed reported that with the approval of the SUS they have been designated one doctor and one nurse, or in some cases a few, that improved the management of the healthcare demand. However, they report these additions are not sufficient and unanimously stressed the need for more human resources. For example, if there is only one odontologist at a health center, no odontologist is present for attending to patients in the afternoon, limiting access to healthcare. Similarly, when doctors are on vacation leave, no one can replace them, with the service being suspended until they return to the office. There is moreover lack of administrative capacity, as often doctors must attend to patients and deal with overburdened administrative procedures. One director reported that sometimes the administrative staff is not properly equipped to deal with procedures that require the use of technology, constituting an additional burden for the already scarce medical staff. As demand has increased, the systems require the provision of more HR designations.
9.5. Quality
Access to healthcare is not only based on geography, organizational availability and affordability, but also on the user's possibility to choose acceptable and effective services. Challenges arising from long waiting times, the limits encountered by chronic patients in accessing services and the difficulties in coordination with other levels of care, among others, substantially lower the quality of public health services. An additional reported challenge comes from the interpersonal nature of relations between providers and users. All interviewed users reported having either experienced bad treatment from a provider or known someone that has. All interviewees stressed the fact that the way one is treated varies widely according to the doctor/nurse encountered on a specific day or at the specific health center. In other words, users report that “not everyone is bad, there are also good doctors and nurses". However, "some just treat us very badly, yell at us, expect us to be knowledgeable of the medical practices and get mad if we do something wrong”, reported one patient outside a second-level hospital. Some users reported that older persons are especially neglected. Furthermore, some reported discrimination related to being indigenous and coming from rural areas, which despite having seen improvements in the last decade, is still visible nowadays. A working paper by ILO (2009), also reported that ethnic origin is an element that generates discrimination and exclusion and is often expressed in a contained demand for cultural reasons (p. 49). The nature of interpersonal relations and discrimination make the services less acceptable for people and might seriously prevent them for seeking healthcare. It also constitutes an infringement of the principle of good treatment proclaimed by Law N° 1152 and restated by Law N° 0132, with the regulation of 2019.
According to users, bad treatment from providers comes probably from the fact that “many providers do not like their professions, that many do it as a business”, otherwise, “they would do their job well and put effort into providing patients with satisfactory outcomes” (Participant 6, personal communication, November, 2021).
Patients also reported that the outcome of the service can be very unsatisfactory Many users report in fact that at public health centers they were told they were perfectly fine, were given some basic medicine and sent home. However, when the visit was repeated with a private doctor, they underwent a complete diagnosis and were prescribed accurate treatment. The consequence of the unsatisfactory service outcome is inevitably patients' skepticism about public providers' level of expertise, especially at the first level of care, and consequently, reluctance to resort anew to public health providers.
Additionally, with the approval of the SUS, a patient must register and attend the health centers corresponding to their residence area. While the regulation aims at ordering access to healthcare, it also accentuates inequalities in availability and quality of services. In fact, people residing in areas with higher quality health centers receive better services, whereas those registered to disadvantaged ones are penalized. In fact, with the case study emerged that there are substantial differences in the quality of healthcare received according to the area in which health centers and hospitals are located. Users interviewed in the Hospitals of Los Pinos and Cotahuma reported quite good experiences, stating that they were treated well and were satisfied with the outcome of the services received. However, users interviewed in La Merced and those that reported having gone to Hospital Holandes reported bad experiences, especially at the latter. Some patients believe that the quality depends on the health center directors and their ability to apply good conduct behavior among their subordinates. Others attribute the deficiencies to a lack of resources assigned to the health establishments. Independently of the causes behind it, healthcare service quality varies considerably among different areas and different hospitals/health centers, exacerbating inequality in access that has for a long time characterized the healthcare system.
Finally, users reported a lack of sufficient information, especially in rural areas, where many are not aware of the existence of the SUS and of the services that it covers. The trend has been confirmed by health center directors, who also reported a lack of sufficient information on the side of patients that reportedly have high expectations as to what the SUS covers, and who are confused by the regulation on the area of registration under the SUS, especially in the first months. In fact, an official from the SUS registration office reported that the government was implementing a socialization plan, traveling across the entire country to provide information to and register uninformed users under SUS.
10. Conclusion
This study's purpose was to provide a general diagnosis of the universal healthcare system, through an analysis of quantitative indicators representative of the national level and a qualitative case study. At the national level, it has been observed that access to public health services has increased compared to previous years. Furthermore, additional human resources and infrastructure have been provided to the public subsector. However, the case study revealed that universal access is limited by several factors. A lack of financial resources leads to a lack of medicines and human resources. Quality-related issues such as long waiting times, perception of low-quality services, and fragile interpersonal relations between users and medical staff constrain access to the services and generate incentives for those who can afford it to seek private healthcare services, resulting in out-of-pocket expenditures despite the formal gratuitous nature of public healthcare services. In other words, the deficiencies that characterized the healthcare system before the approval of the SUS have not improved substantially, while demand and utilization of services have, with consequences for quality and availability Given that the city of La Paz is among the municipalities that receive more resources for healthcare, with one of the highest HDIs in the country (Global Data Lab, 2019), it is unlikely that the results found are outliers. On the contrary, the critical points of access, availability, affordability, and quality identified in La Paz might be exacerbated in areas with fewer resources in the country. The hypothesis is to be verified in future research projects.
Finally, some recommendations for achieving universal healthcare access have been obtained from healthcare providers, users and the wider literature. The most intuitive ones point to increasing the financial resources provided to the healthcare system. Associated with this is the urgency to improve efficiency in spending and in the designation of resources to health establishments and municipalities. Lastly, it is also important to diversify funding sources, as Aponte et al. (2019) have stressed.
Furthermore, health center providers recommend providing them with the required human and physical capacities necessary for attending 80% of the health cases. In fact, health providers and users report that at the present resource level, it is not possible to meet this target. Improving primary attention also means changing the public perception of primary healthcare as being inefficient and unable to provide appropriate diagnosis and treatment.
In addition, the fragile interpersonal relations between providers and users, which was also previously documented, make it necessary to enforce systems of monitoring providers' performance and patients' health outcomes following public service utilization. Generating accountability is fundamental for a high-quality service provision. Lastly, though the contribution of political challenges to low-quality healthcare is rarely acknowledged, it is fundamental to minimize such barriers and self-serving interests in favor of collaboration toward achieving universal healthcare access.